Family Therapies
Individuals are born into families, grow and develop in families, and live most of their lives in families. Therefore, it makes sense that clients are best understood within the context of the family system.
——Dr. Candice Knight, Psychotherapy for the Advanced Practice Psychiatric Nurse
The family system is a social unit that is based on unique relationships and roles. Structural and strategic therapies are important, because they offer unique insights to the theoretical underpinnings of this system. As a psychiatric mental health nurse practitioner, a strong theoretical foundation will help you better understand the family unit and family therapy; this understanding will, in turn, improve the effectiveness of your work with clients.
This week, as you continue exploring family therapy, you examine structural and strategic family therapies and their appropriateness for client families. You also consider your own practicum experiences involving family therapy sessions.
Learning Resources
Note: To access this week’s required library resources, please click on the link to the Course Readings List, found in the Course Materials section of your Syllabus.
Required Readings
Nichols, M. (2014). The essentials of family therapy (6th ed.). Boston, MA: Pearson.
- Chapter 5, “Bowen Family Systems Therapy” (pp. 69–88)
- Chapter 6, “Strategic Family Therapy” (pp. 89–109)
- Chapter 7, “Structural Family Therapy” (pp. 110–128)
Gerlach, P. K. (2015). Use structural maps to manage your family well: Basic premises and examples. Retrieved from http://sfhelp.org/fam/map.htm
McNeil, S. N., Herschberger, J. K., & Nedela, M. N. (2013). Low-income families with potential adolescent gang involvement: A structural community family therapy integration model. American Journal of Family Therapy, 41(2), 110–120. doi:10.1080/01926187.2011.649110
Note: Retrieved from Walden Library databases.
Méndez, N. A., Qureshi, M. E., Carnerio, R., & Hort, F. (2014). The intersection of Facebook and structural family therapy volume 1. American Journal of Family Therapy, 42(2), 167–174. doi:10.1080/01926187.2013.794046
Note: Retrieved from Walden Library databases.
Nichols, M., & Tafuri, S. (2013). Techniques of structural family assessment: A qualitative analysis of how experts promote a systemic perspective. Family Process, 52(2), 207–215. doi:10.1111/famp.12025
Note: Retrieved from Walden Library databases.
Ryan, W. J., Conti, R. P., & Simon, G. M. (2013). Presupposition compatibility facilitates treatment fidelity in therapists learning structural family therapy. American Journal of Family Therapy, 41(5), 403–414. doi:10.1080/01926187.2012.727673
Note: Retrieved from Walden Library databases.
Sheehan, A. H., & Friedlander, M. L. (2015). Therapeutic alliance and retention in brief strategic family therapy: A mixed-methods study. Journal of Marital and Family Therapy, 41(4), 415–427. doi:10.1111/jmft.12113
Note: Retrieved from Walden Library databases.
Szapocznik, J., Muir, J. A., Duff, J. H., Schwartz, S. J., & Brown, C. H. (2015). Brief strategic family therapy: Implementing evidence-based models in community settings. Psychotherapy Research, 25(1), 121–133. doi:10.1080/10503307.2013.856044
Note: Retrieved from Walden Library databases.
Optional Resources
Coatsworth, J. D., Santisteban, D. A., McBride, C. K., & Szapocznik, J. (2001). Brief strategic family therapy versus community control: Engagement, retention, and an exploration of the moderating role of adolescent symptom severity. Family Process, 40(3), 313–332. Retrieved from http://www.familyprocess.org/family-process-journal/
Golden Triad Films (Producer). (1986). The essence of change. [Video file]. Mill Valley, CA: Psychotherapy.net.
National Institute on Drug Abuse. (2003). Brief strategic family therapy for adolescent drug abuse. Retrieved from https://archives.drugabuse.gov/TXManuals/BSFT/BSFTIndex.html
Navarre, S. (1998). Salvador Minuchin’s structural family therapy and its application to multicultural family systems. Issues in Mental Health Nursing, 19(6), 557–570. doi:10.1080/016128498248845
Psychotherapy.net (Producer). (2000b). Satir family therapy [Video file]. Mill Valley, CA: Author.
Psychotherapy.net (Producer). (2011b). Salvador Minuchin on family therapy [Video file]. Mill Valley, CA: Author.
Radohl, T. (2011). Incorporating family into the formula: Family-directed structural therapy for children with serious emotional disturbance. Child & Family Social Work, 16(2), 127–137. doi:10.1111/j.1365-2206.2010.00720.x
Robbins, M. S., Feaster, D. J., Horigian, V. E., Rohrbaugh, M., Shoham, V., Bachrach, K., … Szapocznik, J. (2011). Brief strategic family therapy versus treatment as usual: Results of a multisite randomized trial for substance using adolescents. Journal of Consulting and Clinical Psychology, 79(6), 713–727. doi:10.1037/a0025477
Santisteban, D. A., Suarez-Morales, L., Robbins, M. S., & Szapocznik, J. (2006). Brief strategic family therapy: Lessons learned in efficacy research and challenges to blending research and practice. Family Process, 45(2), 259–271. doi:10.1111/j.1545-5300.2006.00094.x
Szapocznik, J., Schwartz, S. J., Muir, J. A., & Brown, C. H. (2012). Brief strategic family therapy: An intervention to reduce adolescent risk behavior. Couple & Family Psychology, 1(2), 134–145. doi:10.1037/a0029002
Szapocznik, J., Zarate, M., Duff, J., & Muir, J. (2013). Brief strategic family therapy: Engaging drug using/problem behavior adolescents and their families in treatment. Social Work in Public Health, 28(3-4), 206–223. doi:10.1080/19371918.2013.774666
Vetere, A. (2001). Therapy matters: Structural family therapy. Child Psychology & Psychiatry Review, 6(3), 133–139. Retrieved from http://www.iupui.edu/~mswd/D642/multimedia/word_doc/StructuralFamilyTherapy_Vetare.pdf
Weaver, A., Greeno, C. G., Marcus, S. C., Fusco, R. A., Zimmerman, T., & Anderson, C. (2013). Effects of structural family therapy on child and maternal mental health symptomatology. Research on Social Work Practice, 23(3), 294–303. doi:10.1177/1049731512470492
Although structural therapy and strategic therapy are both used in family therapy, these therapeutic approaches have many differences in theory and application. As you assess families and develop treatment plans, you must consider these differences and their potential impact on clients. For this Assignment, as you compare structural and strategic family therapy, consider which therapeutic approach you might use with your own client families.
Learning Objectives
Students will:
- Compare structural family therapy to strategic family therapy
- Create structural family maps
- Justify recommendations for family therapy
To prepare:
- Review this week’s Learning Resources and reflect on the insights they provide on structural and strategic family therapies.
- Refer to Gerlach (2015) in this week’s Learning Resources for guidance on creating a structural family map.
The Assignment
In a 2- to 3-page paper, address the following:
- Summarize the key points of both structural family therapy and strategic family therapy.
- Compare structural family therapy to strategic family therapy, noting the strengths and weaknesses of each.
- Provide an example of a family in your practicum using a structural family map. Note: Be sure to maintain HIPAA regulations.
- Recommend a specific therapy for the family, and justify your choice using the Learning Resources.
SAMPLE ANSWER
Structural versus Strategic Family Therapies
Family therapy is a critical aspect of psychotherapy that helps to investigate changes for the welfare of a family. Psychologists use either strategic or structural therapy when dealing with patients with different issues. Having a better understanding of the models helps psychologists to the best therapy to apply to their customers (Szapocznik et al., 2015). This paper analyzes both structural and strategic therapy as forms of family therapy by discussing their strengths and advantages. The paper also uses a structural family map to give and recommend the best recommendation that will be applicable to the family involved.
ORDER A PLAGIARISM FREE PAPER HERE
The structural family therapy (SFT) is an intervention aimed to address interaction patterns that lead to challenges and issues among family members. The model diagnoses and treats the dysfunction by changing the structure of the family instead of looking to change individual members of the family (Nichols & Tafuri, 2013). It is assumed that problems in the family occur when there is a problem with the hierarchical family structure or when family boundaries are ignored and not met. SFT is critical in maintaining interactions and communications among family members to ensure a healthy healthier family structure (José et al. 2015). Engaging family members can help facilitate change. Changing the family structure can help family members to overcome challenges and interact positively.
The strategic family therapy is more of a problem-solving approach that helps to address dysfunctions within the family. The model aims to influence family members using directives for resolving problems and using carefully planned interventions (Szapocznik et al., 2015). Therefore, the strategic family therapy looks into the strategic way of developing a form of change for each individual in the family. In this way, the underlying problems are recognized and diagnosed to help eliminate negative vibes and unfavorable contacts (Szapocznik et al., 2015). Thus, strategic family therapy uncovers negative feelings within the family and provides ways of engaging destructive behaviors, which encourage positive interactions.
Nursing Paper Help
Both the structural family therapy and strategic family therapy helps to ensure behavioral change, reduce dysfunctional communication, and improve communication among family members. Therefore, both models aim to reduce maladaptive practices that reduce family cohesion to guarantee appropriate family balance (Robbins et al., 2011). However, both structural family therapy and strategic family therapy have disadvantages. The structural family therapy does not primarily look into the issues causing the issues of a dysfunctional family, and it only focuses on interaction and cohesion as the primary form of ensuring the excellent family balance (Nichols & Tafuri, 2013). The strategic family therapy also applies unbalanced techniques during the therapy process such as using a planned and practical form of solving individual family member problems (Robbins et al., 2011). Thus, the models do not use problem-focused form of intervention to address dysfunctional behaviors within the family.
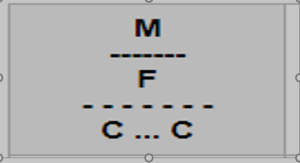
A structural family map can be used as a form of intervention in a family I encountered during my practicum. The family involves Mr. John and Mrs. Mary, where parental communication was minimal, and the woman was dominated. The major conflict within the family was ways of raising their children leading to a mixed-up family hierarchy.
Figure 1: The structural family map.
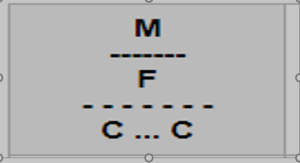
It is recommended that the family should undergo structural family therapy to help improve their communication skills. The therapist should use case-specific creativity by using structural treatment to develop a structural family map for the intervention. Thus, a structural therapy will help build interdependence and communication mechanism between Mr. John and Mrs. Mary because the treatment helps to analyze dysfunctional families and find solution to the underlying issues
References
Nichols, M., & Tafuri, S. (2013). Techniques of structural family assessment: A qualitative analysis of how experts promote a systemic perspective. Family Process, 52(2), 207–215. DOI:10.1111/famp.12025
Ryan, W. J., Conti, R. P., & Simon, G. M. (2013). Presupposition compatibility facilitates treatment fidelity in therapists learning structural family therapy. American Journal of Family Therapy, 41(5), 403–414. DOI:10.1080/01926187.2012.727673
Robbins, M. S., Feaster, D. J., Horigian, V. E., Rohrbaugh, M., Shoham, V., Bachrach, K., … Szapocznik, J. (2011). Brief strategic family therapy versus treatment as usual: Results of a multisite randomized trial for substance-using adolescents. Journal of Consulting and Clinical Psychology, 79(6), 713–727. DOI:10.1037/a0025477
Szapocznik, J., Muir, J. A., Duff, J. H., Schwartz, S. J., & Brown, C. H. (2015). Brief strategic family therapy: Implementing evidence-based models in community settings. Psychotherapy Research, 25(1), 121–133. DOI:10.1080/10503307.2013.856044